Obstructive Sleep Apnea (OSA)
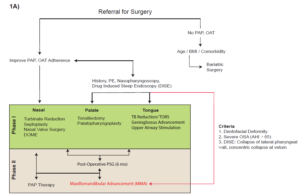
The CRIL has established research and clinical collaboration with OHNS/Sleep Surgery Division at Stanford University. We are currently conducting a retrospective/prospective studies to evaluate the morphological changes in the nasopharyngeal and oropharyngeal airway using CBCT images for different types of skeletal maxillary expansion methods and Maxillomandibular Advancement (MMA) surgery, and their treatment effects on sleep.
Obstructive sleep apnea (OSA) is a condition characterized by repeated episodes of pharyngeal collapse and increased airflow resistance during sleep. Diagnosis of OSA is done through a polysomnogram (PSG) which records physiological measurements, such as arterial oxyhemoglobin desaturation, body position, and inspiratory effort during sleep.
The degree of severity of OSA is quantified by the apnea hypopnea index (AHI), a measure of apneas and hypopnea events per hour of sleep. Up to 25% of adults are thought to have OSA (AHI>5/h), with 10% having moderate to severe disease (>15/h).
OSA is associated with higher rates of cardiovascular and cerebrovascular morbidity and mortality along with excessive daytime sleepiness, fatigue and neurocognitive deficits. If left untreated, the all-cause mortality hazard ratio approaches 4 in patients with severe OSA.
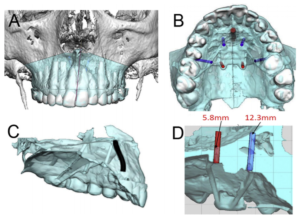
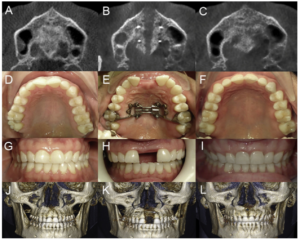
1. Distraction Osteogenesis Maxillary Expansion (DOME) Improves Nasal Breathing and OSA
- Distraction Osteogenesis Maxillary Expansion (DOME) for adult obstructive sleep apnea patients with narrow maxilla and nasal floor. Audrey Yoon, Christian Guilleminault, Soroush Zaghi, Stanley Yung-Chuan Liu. Sleep Med. 2020 Jan;65:172-176.
- This study correlates objective and subjective measurements associated with obstructive sleep apnea (OSA) to define the efficacy of Distraction Osteogenesis Maxillary Expansion (DOME) to treat adult OSA patients with narrow maxilla and nasal floor.
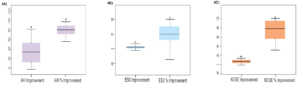
- The mean age of test subjects was 30.5 ± 8.5 years with a gender distribution of 57 males and 18 females. There was a significant reduction in pre- and post-operative NOSE score (10.94 ± 5.51 to 3.28 ± 2.89, p< 0.0001), mean ESS score (10.48 ± 5.4 to 6.69 ± 4.75, p< 0.0001), and AHI (17.65 ± 19.30 to 8.17 ± 8.47, p < 0.0001) with an increased percentage of REM sleep (14.4 ± 8.3% to 22.7 ± 6.6%, p = 0.0014). No significant adverse effects were identified.
- DOME treatment reduced the severity of OSA, refractory nasal obstruction, daytime somnolence, and increased the percentage of REM sleep in this selected cohort of adults OSA patients with narrow maxilla and nasal floor.
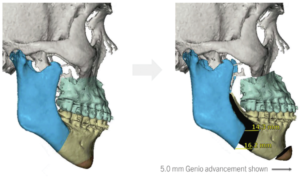
2. OSA and Maxillomandibular Advancement (MMA) Surgery
- Maxillomandibular advancement (MMA) was developed in the mid 1980’s as a surgical approach to significantly increase the soft tissue pharyngeal space by expanding the skeletal framework, resulting in reduced pharyngeal collapse during inspiration.
- MMA is considered the most effective craniofacial surgical technique for the treatment of OSA in adults. The largest systematic review and meta-analysis of MMA revealed that of the 627 subjects in 22 different patient centers, the pooled success and cure rates were 86% and 43.2%, respectively.
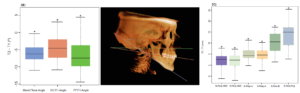
- The purpose of the study was to evaluate the effects of maxillomandibular advancement (MMA) surgery on skeletal and dental landmarks and to determine any correlations with obstructive sleep apnea (OSA).
- Mean AHI improvement was 38.49 events/hr which demonstrated a 74.91% improvement following MMA. Surgical success criteria was defined as postoperative AHI reduction to < 20 events/hr and >50% reduction in postoperative AHI reduction to < 20 events/hr and > 50% reduction in postoperative AHI (Sher). From this criteria, 13 out of the 15 subjects had a successful outcome.
- MMA results in:
-
- a significant change in the maxillary and mandibular sagittal position
- greater change in the mandible sagittal position than the maxillary sagittal position
- a significant maxillary and mandibular CCW rotation
- MMA yields a statistically significant improvement in AHI and clinically significant improvement in ESS and NOSE scores.